Our most recent projects
January 2026
Contribution to the leprosy research department of Netherlands Leprosy Relief, 2026 The Turing Foundation has been co-financing projects related to the fight against leprosy with Netherlands Leprosy Relief for years.
On top of this, every year we also donate directly to Netherlands Leprosy Relief
as a contribution towards the overhead costs it incurs as a... more
January 2026
Evaluation of five transcriptomic biomarkers for leprosy, Colombia, 2026-2027 Approximately 400 of the leprosy cases reported each year in the world are from Colombia.
In this project of the Instituto Colombiano de Medicina Tropical,
researchers in the five regions with the highest incidence of leprosy in Colombia are taking samples from cases,
their close... more
October 2025
Extra clofazimine for MB cases at high risk of ENL reactions, 2025-2027 Erythema Nodosum Leprosum (ENL) is a serious and very painful leprosy complication. The disease can be treated with the drug clofazimine. This research project aims to evaluate whether treating leprosy patients with extra clofazimin reduces the severity and frequency of ENL and whether it... more
October 2025
MetLep Trial: Metformin as adjunct therapy for MB leprosy, 2025-2026 Metformin is a cheap and safe medicine which has been used to treat diabetes for a long time. Research into tuberculosis patients, which is caused by a bacterium similar to leprosy, has demonstrated that metformin has a beneficial effect on the immune system. The IOCRL (Universities of... more
October 2025
ENLIST Randomised controlled trials of methotrexate in Erythema Nodosum Leprosum, 2025-2026 Erythema Nodosum Leprosum (ENL) is a serious and very painful leprosy complication. It is often chronic and causes serious morbidity, not only affecting the skin but also bones, joints, eyes, nerves, testes, and kidneys. Effective treatment for ENL is available but... more
October 2025
Immunomodulation by Mycobacterium Indicus Pranii (MIP) in MB leprosy, 2025 Leprosy patients can be effectively treated with multi-drug treatment (MDT), but they are still susceptible to being reinfected with leprosy. It has been demonstrated that the MIP (Mycobacterium indicus pranii) vaccine can teach the immune system to activate an immune response when it... more
July 2025
Use of handheld ultrasound for the early detection of leprosy, India en Nepal, 2025-2026 Early detection of leprosy is important to ensure treatment starts before the disease progresses and other people are infected.
Leprosy symptoms are now often diagnosed "by hand and eye" registrations. However, ultrasound scans provide a quick and more accurate
results... more
July 2025
Role of drug resistance and M. lepromatosis in African leprosy transmission, Burundi, Cameroon, D.R. Congo, Ghana, België, 2025-2027 In a number of African countries leprosy is still discovered relatively late during which the disease has already advanced.
In addition, there is no research conducted in Central Africa to investigate the resistance to... more
July 2025
Leprosy transmission and One Health. Holistic investigation for environmental presence of Mycobaterium leprae, India, 2025-2027 Leprosy infections are known to spread from person to person, but leprosy bacteria have also been found in certain animals,
in water, and in the soil. Till date it is not clear whether contamination can also occur via these... more
May 2025
ENL Genomic Signature and Neutrophil Interventions, Brazilië, 2025-2028 Patients with lepromatous leprosy and borderline leprosy can develop a severe immunological complication known as Erythema Nodosum Leprosum (ENL). This reaction can affect patients even after completing treatment and may lead to nerve damage and dysfunction. To treat ENL episodes,... more
May 2025
PUCP, Genetic susceptibility to leprosy and disease recurrence, 2025-2027 Development of a leprosy infection into the disease is strongly dependent on a patient's genetic makeup. Technological innovations have enabled DNA-related studies to successfully identify various candidate genes associated with leprosy transmission as well as with clinical... more
|
Submit an application?
The Turing Foundation supports only leprosy control applications
related to scientific research, particularly into early diagnosis.
If your project meets our criteria, your application is most welcome.
Read more
|
Our scientific research projects
 |
Contribution to the leprosy research department of Netherlands Leprosy Relief, 2026
The Turing Foundation has been co-financing projects related to the fight against leprosy with Netherlands Leprosy Relief for years.
On top of this, every year we also donate directly to Netherlands Leprosy Relief
as a contribution towards the overhead costs it incurs as a member of the Leprosy Research Initiative:
the international partnership for financing leprosy research.
Our 2026 contribution towards Netherlands Leprosy Relief's overhead costs has been set at € 20.000.
See also:

Bijdrage aan de wetenschapstak van de Leprastichting
|
  |
ENLIST Randomised controlled trials of methotrexate in Erythema Nodosum Leprosum, 2025-2026
Erythema Nodosum Leprosum (ENL) is a serious and very painful leprosy complication. It is often chronic and causes serious morbidity, not only affecting the skin but also bones, joints, eyes, nerves, testes, and kidneys. Effective treatment for ENL is available but expensive, has considerable side-effects, and is often inaccessible in many countries where leprosy is endemic.
Methotrexate is cheap and has been used all over the world to treat conditions like psoriasis since the 1950s. This medicine is possibly an effective alternative to prednisolone (the most widely used corticosteroid treatment for ENL). The London School of Hygiene and Tropical Medicine will validate this by inviting patients with ENL in Bangladesh, Brazil, Ethiopia, India, Indonesia, Nepal and the Philippines to take part in a study where some patients are prescribed methotrexate, and others prednisolone.
The Turing Foundation is contributing €350,000 towards this research
See also:

Randomised controlled trials of methotrexate in Erythema Nodosum Leprosum
|
  |
Use of handheld ultrasound for the early detection of leprosy, India en Nepal, 2025-2026
Early detection of leprosy is important to ensure treatment starts before the disease progresses and other people are infected.
Leprosy symptoms are now often diagnosed "by hand and eye" registrations. However, ultrasound scans provide a quick and more accurate
results and is cheap. Nonetheless, this requires large equipment which is not available everywhere.
American Leprosy Missions investigates whether a recently developed portable ultrasound device can detect leprosy symptoms as
accurately (and possibly detect changes after treatment has started).
The Turing Foundation is contributing €57,974 to this project.
The Leprosy Research Initiative contributes the same amount.
See also:

Use of handheld ultrasound for the early detection of leprosy, India en Nepal
|
  |
Role of drug resistance and M. lepromatosis in African leprosy transmission, Burundi, Cameroon, D.R. Congo, Ghana, België, 2025-2027
In a number of African countries leprosy is still discovered relatively late during which the disease has already advanced.
In addition, there is no research conducted in Central Africa to investigate the resistance to antibiotics in standard leprosy treatments.
Lastly, there are no insights into the possible presence of M. lepromatosis, a bacterium related to M. leprae that also causes leprosy.
Institute of Tropical Medicine Antwerp researches in Burundi, Cameroon, D.R. Congo and Ghana the presence,
quantity and resistance of the two bacteria at infected patients. The entire genome of the bacterium is being examined,
which may also enable new biomarkers to be found that could demonstrate resistance. The research provides insight into how
the bacteria changes and spreads.
The Turing Foundation is contributing €160,408 to this project (of which €37,197 in 2025).
The Leprosy Research Initiative contributes the same amount.
See also:

Role of drug resistance and M. lepromatosis in African leprosy transmission
|
  |
Leprosy transmission and One Health. Holistic investigation for environmental presence of Mycobaterium leprae, India, 2025-2027
Leprosy infections are known to spread from person to person, but leprosy bacteria have also been found in certain animals,
in water, and in the soil. Till date it is not clear whether contamination can also occur via these bacteria.
LEPRA Society - Blue Peter Public Health and Research Center
investigates the link between leprosy cases and their exposure to livestock, water and soil in four villages in India. If the presence of leprosy bacteria in open water, wastewater, soil and/or livestock is identified together with a link to the leprosy cases, a stronger strategy against leprosy and leprosy transmission can be developed.
The Turing Foundation is contributing €100,466 to this project (of which €35,484 in 2025).
The Leprosy Research Initiative contributes the same amount.
See also:

Holistic investigation for environmental presence of Mycobacterium leprae and its implications in leprosy transmission
|
  |
ENL Genomic Signature and Neutrophil Interventions, Brazilië, 2025-2028
Patients with lepromatous leprosy and borderline leprosy can develop a severe immunological complication known as Erythema Nodosum Leprosum (ENL). This reaction can affect patients even after completing treatment and may lead to nerve damage and dysfunction. To treat ENL episodes, immunosuppressive medications are used to suppress the excessive inflammatory response, often requiring prolonged use of corticosteroids and/or thalidomide. However, these medications can cause serious side effects.
Thalidomide is highly effective in alleviating ENL symptoms, often within a few days, but its teratogenic properties (which can cause birth defects in foetuses) restrict its use to people outside reproductive age. As a result, the drug is only approved for use in certain countries, such as India and Brazil. Although it is believed that the immune system-modulating effects of thalidomide make it effective in treating ENL, the exact molecular targets in ENL are not yet fully understood.
In recent studies, researchers have analysed how our genes respond to infections, with a focus on ENL. Genes from leprosy patients with and without ENL were compared, also with patients starting thalidomide treatment. Previously, the researchers studied the genes in skin lesions of ENL patients and discovered certain genes associated with a kind of white blood cell, neutrophils. Now, the Oswaldo Cruz Foundation aims to identify the opposite gene pattern, hoping that this will lead to new targeted treatments for ENL.
The researchers plan computer analyses to identify drugs that can influence these genes and will then test them in the laboratory using neutrophils from healthy people and leprosy patients, with or without ENL. By providing more insight into the progression of the disease and immunology, the research will contribute to the development of more effective treatment strategies for ENL. This will lead to a quicker start of treatment and better outcomes for affected individuals.
The Turing Foundation is contributing €86,619 towards this project (of which €27,000 in 2025).
See also:

ENL Genomic Signature and Neutrophil Interventions
|
  |
PUCP, Genetic susceptibility to leprosy and disease recurrence, 2025-2027
Development of a leprosy infection into the disease is strongly dependent on a patient's genetic makeup. Technological innovations have enabled DNA-related studies to successfully identify various candidate genes associated with leprosy transmission as well as with clinical manifestations of the disease, including the type of leprosy and the occurrence of leprosy reactions. However, only a few of these studies have focused on accurately identifying the actual causal genetic variants of the disease. Moreover, recurrence of leprosy (due to relapse or reinfection) is an under-researched phenomenon, despite its significant impact on healthcare systems. The research team has already identified many genetic variants with potentially strong effects on leprosy; they have also described a genetic profile that could indicate hyper-susceptibility in patients who have experienced recurrence of the disease. The next step is to validate these results in different populations.
In this project, Pontifícia Universidade Católica do Paraná (PUCP) researchers will search for new genetic variants associated with leprosy and will verify these variants using a large sample of the Brazilian population. The researchers will analyse the impact of these variants together to describe a genetic profile that may make patients more susceptible to developing leprosy, even after a previous infection. Finally, they hope to contribute to the development of a genetic panel that can be used to monitor patients and their contacts, particularly in endemic areas.
The Turing Foundation is contributing €39,432 towards this project.
See also:

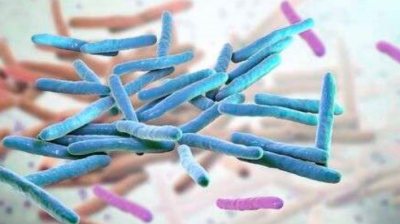
Scanning Electron Microscopy of M. leprae
|
 |
Contribution to the leprosy research department of Netherlands Leprosy Relief, 2025
The Turing Foundation has been co-financing projects related to the fight against leprosy with Netherlands Leprosy Relief for years.
On top of this, every year we also donate directly to Netherlands Leprosy Relief
as a contribution towards the overhead costs it incurs as a member of the Leprosy Research Initiative:
the international partnership for financing leprosy research.
Our 2025 contribution towards Netherlands Leprosy Relief's overhead costs has been set at € 20.000.
See also:

Bijdrage aan de wetenschapstak van de Leprastichting
|
  |
Mobile suitcase lab for rapid diagnosis of clinical and sub-clinical leprosy, Bangladesh, 2025
Early diagnosis of leprosy is crucial for effective treatment of cases and preventing infection of their close contacts, who are the group most at risk. Microbiological diagnosis of leprosy outside well-equipped laboratories with specifically trained personnel is difficult. This project focuses on a reliable, simple and cost-effective rapid diagnostic test, which is easy to use and can be used on the ground.
A molecular diagnostic test, the ML-RPA test, has already been developed for this purpose. This rapid diagnostic test provides results within 20 minutes and proved very accurate in previous studies using laboratory-grown DNA. The test is conducted in a 'mobile suitcase lab' to research the effectiveness of diagnosis of leprosy cases and their close contacts on the ground. The suitcase lab is easily transportable, uses solar panels and a portable charger, and does not have to be cooled. The ML-RPA test is compared to an RT-PCR test (which is also a molecular diagnostic test able to detect the leprosy bacteria accurately). The results of the two tests are being compared and if the ML-RPA test shows comparable or greater accuracy than the RT-PCR test then it will be recommended for difficult cases and their contacts, especially in areas lacking a good laboratory.
The Turing Foundation is contributing € 30,000 towards this project.
See also:

M. Leprae bacteria
|
More projects
| |
|
| |