Projects in India
|
 |
Immunomodulation by Mycobacterium Indicus Pranii (MIP) in MB leprosy, 2020-2025
Leprosy patients can be effectively treated with multi-drug treatment (MDT), but they are still susceptible to being reinfected with leprosy. It has been demonstrated that the MIP (Mycobacterium indicus pranii) vaccine can teach the immune system to activate an immune response when it encounters M. leprae. This process is called 'immune modulation'. The National Institute of Research in Tribal Health (ICMR) in India uses advanced techniques to investigate the cells involved in an immune response and the differences between MIP-vaccinated and unvaccinated patients. The research aims to better understand the underlying mechanism of immune response and immune modulation, and use the knowledge gained to fight leprosy more effectively. The Turing Foundation is contributing € 94,000 towards this project. See also:  M. Leprae bacterie |
|
ENLIST Randomised controlled trials of methotrexate in Erythema Nodosum Leprosum, 2016-2026
Erythema Nodosum Leprosum (ENL) is a serious and very painful leprosy complication. It is often chronic and causes serious morbidity, not only affecting the skin but also bones, joints, eyes, nerves, testes, and kidneys. Effective treatment for ENL is available but expensive, has considerable side-effects, and is often inaccessible in many countries where leprosy is endemic. Methotrexate is cheap and has been used all over the world to treat conditions like psoriasis since the 1950s. This medicine is possibly an effective alternative to prednisolone (the most widely used corticosteroid treatment for ENL). The London School of Hygiene and Tropical Medicine will validate this by inviting patients with ENL in Bangladesh, Brazil, Ethiopia, India, Indonesia, Nepal and the Philippines to take part in a study where some patients are prescribed methotrexate, and others prednisolone. The Turing Foundation is contributing €350,000 towards this research See also:
Leprosy Research Initiative: other projects
Other projects in Brazil
Other projects in Ethiopia
Other projects in Bangladesh
Other projects in Indonesia
Other projects in Nepal
Other projects in Philippines
 Randomised controlled trials of methotrexate in Erythema Nodosum Leprosum |
 |
Extra clofazimine for MB cases at high risk of ENL reactions, Bangladesh en India, 2020-2027
Erythema Nodosum Leprosum (ENL) is a serious and very painful leprosy complication. The disease can be treated with the drug clofazimine. This research project aims to evaluate whether treating leprosy patients with extra clofazimin reduces the severity and frequency of ENL and whether it prevents nerve damage over a 24-month period. The Bombay Leprosy Project research is being conducted in Bangladesh and India. The Turing Foundation is contributing € 100,000 towards this project. See also: 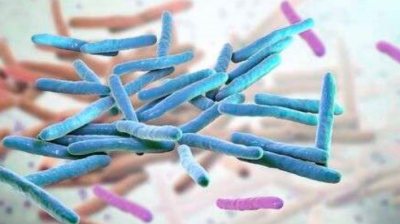 M. Leprae bacterie |
|
Use of handheld ultrasound for the early detection of leprosy, India en Nepal, 2024-2026
Early detection of leprosy is important to ensure treatment starts before the disease progresses and other people are infected. Leprosy symptoms are now often diagnosed "by hand and eye" registrations. However, ultrasound scans provide a quick and more accurate results and is cheap. Nonetheless, this requires large equipment which is not available everywhere. American Leprosy Missions investigates whether a recently developed portable ultrasound device can detect leprosy symptoms as accurately (and possibly detect changes after treatment has started). The Turing Foundation is contributing €57,974 to this project. The Leprosy Research Initiative contributes the same amount. See also:
America Leprosy Missions: other projects
Leprosy Research Initiative: other projects
Other projects in Nepal
 Use of handheld ultrasound for the early detection of leprosy, India en Nepal |
 |
Leprosy transmission and One Health. Holistic investigation for environmental presence of Mycobaterium leprae, India, 2024-2027
Leprosy infections are known to spread from person to person, but leprosy bacteria have also been found in certain animals, in water, and in the soil. Till date it is not clear whether contamination can also occur via these bacteria. LEPRA Society - Blue Peter Public Health and Research Center investigates the link between leprosy cases and their exposure to livestock, water and soil in four villages in India. If the presence of leprosy bacteria in open water, wastewater, soil and/or livestock is identified together with a link to the leprosy cases, a stronger strategy against leprosy and leprosy transmission can be developed. The Turing Foundation is contributing €100,466 to this project (of which €35,484 in 2025). The Leprosy Research Initiative contributes the same amount. See also:  Holistic investigation for environmental presence of Mycobacterium leprae and its implications in leprosy transmission |
 |
Research on treatment of early neuropathy in leprosy 2014-2017
The TENLEP Research Consortium (Treatment of Early Neuropathy in Leprosy) is a large international association in which 14 researchers from renowned research institutes all over the world work together, combining their expertise in the field of leprosy-related inflammation of the nerves. TENLEP Trial is a large-scale research project focussing on nerve damage caused by leprosy. Its central research questions are: 2. What is the most effective treatment for patients who have a clinical nerve function impairments? See also:
Other projects in Indonesia
Other projects in Bangladesh
Other projects in Philippines
Other projects in Brazil
Other projects in Ethiopia
 Scanning Electron Microscopy of M. leprae |
  |
Education for 250 street children in Calcutta, India, 2007-2009
The Partnership Foundation is devoted to providing accommodation for street children in India in existing school buildings. The Loreto Sealdah Day School in Calcutta serves as a model for this strategy. It is a high-quality private school for 1,500 girls. A so-called 'Rainbow Home' is being created in this school. The home can accommodate 250 street children and provides them with food, education, medical care and loving support. Since 2007, the Turing Foundation covers the full educational costs of the project, amounting to € 56,000 in 2009.  Rainbow Home, Calcutta |



















